Please review the following guidelines for in-hospital management for all North American pit vipers. Pit vipers in the United States include all rattlesnakes, copperheads, and cottonmouths (also known as water moccasins). You do not need to identify the species of snake in order to treat in the USA as both CroFab and Anavip are both FDA approved for all North American pit viper envenomations. While antivenom is most effective in the first six hours, it can still benefit if there are ongoing venom effects.
Pit viper envenomation is GENERALLY characterized by local tissue injury and, less commonly, hematologic abnormalities and systemic toxicity such as low blood pressure, vomiting, airway swelling. Some pit vipers, such as certain populations of Mojave rattlesnakes, cause neurological toxicity.
The most important steps to be taken in-hospital:
Keep the affected extremity elevated.
Make sure they check the following laboratory tests: CBC, BMP, PT/INR, Fibrinogen, CK.
Ask them what their indications for antivenom are, and make sure they are consistent with what we have mentioned here:
Significant or progressive local tissue damage; e.g., tenderness and swelling that crosses one major joint, hemorrhagic bleb
Hematologic toxicity; e.g., PT >15s, fibrinogen <150mg/dL, platelets <150K/µL
Systemic toxicity; e.g., hypotension, airway swelling, neurological toxicity
If you do not feel you're getting appropriate care, advocate for yourself. Request they involve an expert. If necessary, request transfer to a more appropriate facility.
Do not agree to prophylactic antibiotics or prophylactic surgical intervention.
You do not need to identify the snake in order to receive antivenom. CroFab and Anavip are both FDA approved to treat all North American pit vipers. Pit vipers include rattlesnakes, copperheads, and cottonmouths (aka water moccasins).
Click for the BMC Emergency Medicine Unified Treatment Algorithm for the Management of Crotaline Snakebites in the United Statesand flowchart for your physician to review.
Algorithms & Guidelines
-

NSS In-Hospital Management
-
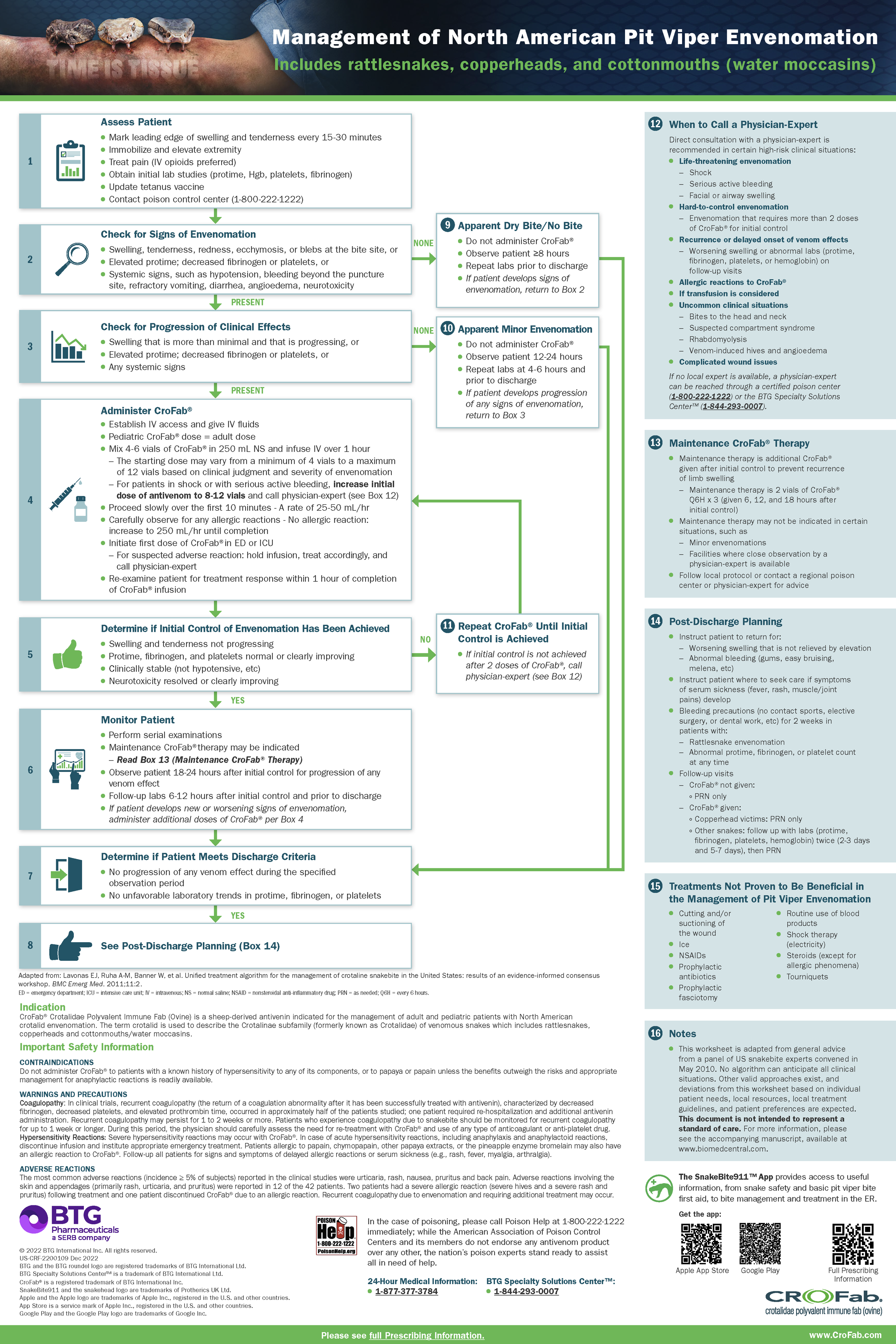
CroFab Algorithm
View all CroFab’s resources including an interactive algorithm and full treatment algorithm research article at https://crofab.com/envenomation-education/treatment-algorithm.html?gad_source=1
-

Anavip Algorithm
Download the the pdf format here.
View all Anavip’s resources including the treatment algorithm, package insert, and product information at https://anavip-us.com/downloads/
-
Written by Dr. Spencer Greene, MD, MS, FACEP, FACMT, FAACT, FAAEM
Not all pit viper bites result in envenomation. In about 10% to 15% of bites that present to the emergency department, no venom was delivered. We call this a dry bite. Because no venom is delivered, there will be minimal signs and symptoms. It’s essentially the same as getting pricked by a thumbtack.
IF A PATIENT IS HAVING BRUISING, SWELLING, PAIN, ETC., IT INDICATES THERE HAS BEEN AN ENVENOMATION AND IS THEREFORE NOT A DRY BITE. The absence of lab abnormalities does not mean it’s a dry bite.
Snakebites are a dynamic process. The diagnosis of dry bite cannot be made after 30 minutes of observation. Not even two hours. Not even four hours. Patients who may have been bitten by a venomous snake should be observed for AT LEAST eight hours. If there are no local findings, no systemic toxicity, and no hematologic lab abnormalities, then it is reasonable to make the diagnosis of a dry bite. To call it a dry bite after one hour of observation is a recipe for disaster and has resulted in some pretty expensive lawsuits.
This observation is emphasized in the unified treatment algorithm, which you can read here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3042971/
-
Written by Dr. Spencer Greene, MD, MS, FACEP, FACMT, FAACT, FAAEM
Kids can receive antivenom, and we DO NOT ADJUST THE DOSE. You’re not really treating the patient, but rather the venom. In a pediatric snakebite victim, the ratio of venom to body weight is actually higher, so you do not give a smaller antivenom dose than you would use in an adult. Start with the same dose, and give additional antivenom if the child is not improving as expected. In very small children, the antivenom can be prepared in a more concentrated form to prevent volume overload.
-
Written by Dr. Spencer Greene, MD, MS, FACEP, FACMT, FAACT, FAAEM
When determining how to position the affected extremity following a snakebite, there are two things to consider: (1) the type of snake, and (2) whether you’re already at the hospital or still in the pre-hospital environment.
Experts agree that crotalid (copperhead, cottonmouth, rattlesnake) envenomations should be ELEVATED in the hospital. Elevate the extremity at least 45° (ideally at least 60°) without allowing the knee or elbow to bend. It’s one of the first recommendations in the unified treatment algorithm for the management of crotaline snakebite in the U.S.: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3042971/
Pre-hospital positioning is a little controversial. Some people recommend keeping the affected extremity at heart level because they fear that elevation will increase the systemic absorption of the venom. Dr. Greene recommends early and aggressive elevation, because the volume of venom is so insignificant that elevation is unlikely to make a difference in absorption. On the other hand, the volume of fluids that accumulate in the affected extremity is significant, and elevation will reduce that swelling. He reports seeing dramatic improvement within 30 minutes of elevation.
The affected extremity should never be placed below heart level. This will increase the swelling and hydrostatic pressures that lead to tissue injury.
Coral snake envenomations do not cause significant swelling, and we recommend patients placing the affected extremity in whatever position is most comfortable.
You can read Dr. Greene’s article here:
https://medium.com/natural-world/how-to-position-a-snakebite-9430fc988af
https://btgsp.com/en-us/insights/don-t-just-do-something-stand-there
-
Written by Dr. Spencer Greene, MD, MS, FACEP, FACMT, FAACT, FAAEM
Pit viper bites can cause serious obstetrical complications in pregnancy, including fetal death. Pregnant patients may receive antivenom. The best way to protect the fetus is by treating the mother.
Additional reading from Asclepius Snakebite Foundation.
https://www.snakebitefoundation.org/blog/what-to-expect-when-youre-expecting-and-snakebitten
-
Written by Dr. Spencer Greene, MD, MS, FACEP, FACMT, FAACT, FAAEM
Although antivenom is most beneficial when started within the first 6 hours, it can provide benefit even when started several days later. We sometimes dose patients with antivenom even one week after a bite. If there are ongoing venom effects, antivenom should be administered, or at least considered.
-
Written by Dr. Spencer Greene, MD, MS, FACEP, FACMT, FAACT, FAAEM
Copperhead envenomations should be treated like other native crotalid envenomations. Although the average copperhead envenomation tends to be less severe than a typical rattlesnake envenomation, any native crotalid envenomation can result in significant local and systemic toxicity. Furthermore, many snakes go unseen, and among those that are observed, misidentification is common.
A randomized clinical trial demonstrated that even mild copperhead envenomations recover more quickly when treated with CroFab compared to placebo. CroFab also reduced total opioid requirements. As the severity of the envenomation increases, the benefits of antivenom are increasingly apparent.
Randomized clinical trial of CroFab for copperhead envenomations: https://pubmed.ncbi.nlm.nih.gov/28601268/
Early antivenom administration accelerates recovery: https://pubmed.ncbi.nlm.nih.gov/30175628/
Antivenom reduces opioid requirements: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6526891/Item description
